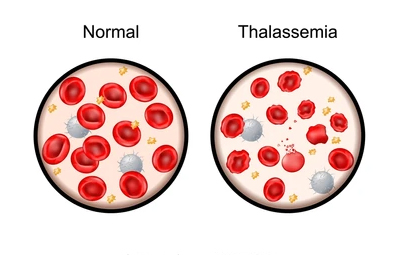
Children with Transfusion-Dependent Thalassemia (TDT) cannot produce enough healthy hemoglobin. Regular transfusions maintain hemoglobin at 9–10.5 g/dL, supporting growth, brain development, and heart health.
Most children need blood every 3–4 weeks. The schedule may vary slightly based on growth, illness, and pre-transfusion hemoglobin.
Every child with thalassemia should receive:
Fever, chills, rashes, difficulty breathing, dark urine, vomiting, or back pain. Report immediately.
Each transfusion adds iron that accumulates in organs. Excess iron affects the heart, liver, hormones, and bones. Chelation therapy (Deferasirox, Deferiprone, Deferoxamine) removes excess iron.
Maintain a transfusion diary, track hemoglobin, hydrate well, continue normal activities and school whenever possible.
Stem Cell Transplant (HSCT) and gene therapy are the only curative treatments.