A Pediatric Hematopoietic Stem Cell Transplant (HSCT), commonly known as a bone marrow transplant, is a transformative treatment that can cure many serious childhood illnesses. These include blood cancers like leukemia, inherited blood disorders such as thalassemia and sickle cell disease, severe immune deficiencies, and some metabolic disorders. Although the name sounds complicated, the concept is simple: replace unhealthy blood-forming cells with healthy ones so the child’s body can start making normal blood again.
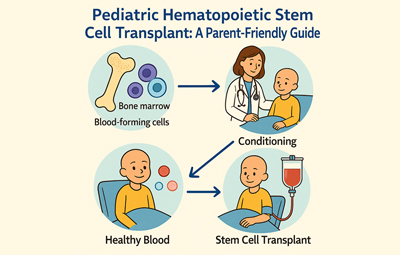
Stem cells live inside the bone marrow and produce red cells, white cells, and platelets—each crucial for carrying oxygen, fighting infections, and preventing bleeding. When these stem cells stop working properly, the child may need new ones. These healthy stem cells can come from the child (autologous transplant) or from a donor such as a sibling, parent, or a matched volunteer (allogeneic transplant).
Before receiving the new cells, the child undergoes “conditioning”—a carefully planned set of medicines that clears out diseased cells and prepares the body to accept the transplant. The transplant itself is not a surgery. It is simply a drip of stem cells through a vein, very similar to receiving a blood transfusion. Over the next few weeks, these cells travel to the bone marrow and begin producing healthy blood.
The recovery period requires close care because the child’s immunity is temporarily low. Doctors monitor for infections and possible complications, all of which are manageable with modern treatments. Today, HSCT outcomes are better than ever, giving thousands of children each year a chance at a healthier, fuller life.
With medical advances, strong family support, and expert care teams, HSCT offers real hope—and often a cure—for children facing some of the toughest diseases.